In a current evaluation revealed within the journal Current Opinion in Chemical Biology, researchers mentioned the newest advances within the antimicrobial properties of human milk.
Evaluation: Recent advances on human milk oligosaccharide antimicrobial activity. Picture Credit score: HTeam / Shutterstock
Background
Human breastmilk is the one dietary supply really useful in the course of the first months of a new child’s life. Nevertheless, globally, solely 40% of infants underneath six months obtain breastmilk as their sole dietary supply. A number of elements contribute to the noticed breastfeeding price, comparable to metabolic problems within the new child, maternal well being problems stopping lactation or secure breastfeeding, and insufficient assist for moms.
Breastmilk consists of a number of antimicrobial, anti-inflammatory, and immunomodulatory molecules, which assist to decrease toddler morbidity, set up the microbiome, and facilitate psychomotor and cognitive improvement. Infants turn into inclined to well being points within the absence of human milk. Within the current research, researchers reviewed the antimicrobial exercise of human milk oligosaccharides (HMOs).
HMOs differ in composition
Structurally, HMOs include 5 pyranoses – D-glucose, D-galactose, D-N-acetylglucosamine, N-acetylneuraminic acid, and L-fucose. Every oligosaccharide incorporates lactose on the lowering finish. Up to now, 200 distinctive HMOs incorporating 3 – 22 monosaccharides have been characterised. The composition of HMOs is variable amongst moms and adjustments all through lactation. The focus of HMOs over the course of lactations ranges from 5 g/L to 25 g/L.
Human milk composition adjustments as per the toddler’s physiological necessities. The primary milk (colostrum) is produced after childbirth for as much as seven days. It’s nearly non-nutritious and primarily helps to ascertain immunity. By the fourth week, the neonatal food plan contains mature breast milk. HMOs attain peak concentrations throughout this early part. Though moms spend round 300 to 500 energy to synthesize HMOs, they don’t seem to be metabolized and are as a substitute used for commensal micro organism as a carbon supply.
The intestine microbiome of non-breastfed neonates is completely different from these of breastfed. Toddler formula-fed kids exhibit larger microbiota variety, whereas these breastfed have microbiotas dominated by the probiotic Bifidobacterium. Within the later lactation levels, Bacteroides dominate the microbiome.
Antibacterial exercise of HMOs
Streptococcus agalactiae, a gaggle B Streptococcus (GBS) and a gram-positive pathogen, colonizes the vaginal tract of roughly 15% to 30% of wholesome females. It could possibly be vertically transmitted and causes neonatal meningitis and sepsis. Western international locations have devised methods to stop its transmission by implementing prenatal screening for GBS, adopted by antibiotic prophylaxis.
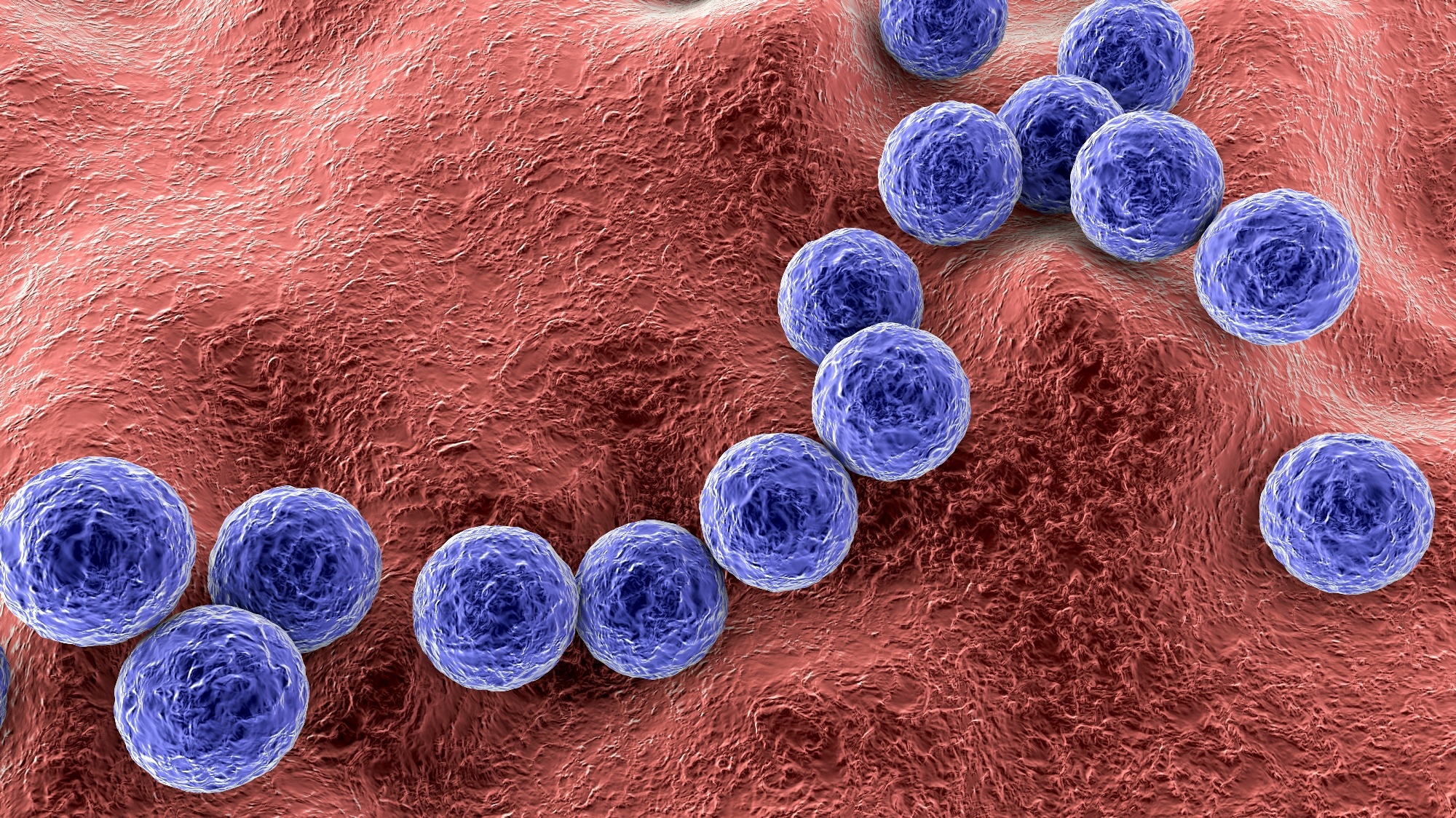 Gram-positive micro organism Streptococcus agalactiae. Picture Credit score: Kateryna Kon / Shutterstock
Gram-positive micro organism Streptococcus agalactiae. Picture Credit score: Kateryna Kon / Shutterstock
Though the charges of early onset of GBS an infection are diminished with this strategy, there isn’t any prophylactic or healing remedy for late-onset illness. As a substitute, researchers explored the antimicrobial properties of HMOs in opposition to GBS. One research supported the antimicrobial exercise of HMOs in opposition to GBS and famous that therapy with heterogeneous HMOs had not affected the composition of vaginal microbiota no matter GBS an infection.
HMOs inhibit biofilm formation
Bacterial biofilms are mobile aggregates enclosed in a dynamic and inflexible extracellular matrix (ECM), which assist microbes to coordinate in a group. The ECM confers safety from antibiotics, resulting in antibiotic tolerance usually related to antimicrobial resistance (AMR). HMOs act as receptor decoys to inhibit the attachment of pathogens to mucosal surfaces. Staphylococcus aureus colonizes the pores and skin and nasopharynx of 30% of the inhabitants.
It’s an opportunistic pathogen that normally presents asymptomatically however is chargeable for a number of medical manifestations as soon as it establishes pathogenicity. These micro organism are recognized to provide biofilms. The research’s authors have beforehand reported using HMOs to disrupt bacterial attachment to abiotic and biotic surfaces. They reported that HMOs may considerably inhibit the formation of S. aureus biofilms.
Furthermore, synthetically modified HMOs demonstrated an elevated inhibitory impact on biofilm formation. One other research noticed diminished viability of bacterial cells inside S. aureus biofilms, suggestive of cell demise. Enteropathogenic Escherichia coli (EPEC) is a gaggle of E. coli serotypes and recognized contaminants of water and meals.
EPEC attaches to the intestinal epithelium and kinds distinct colonies. In a research, researchers discovered that in vitro supplementation of HMOs to tradition media had considerably decreased attachment of EPEC. Acinetobacter baumannii, a gram-negative species, is extensively recognized for multi-drug resistance (MDR). A. baumannii infections happen in intensive care models (ICUs), the place sufferers are immunocompromised.
A. baumannii causes ventilator-acquired pneumonia (VAP), the place infections are acquired from its biofilms on ventilator gear. The research’s authors investigated the applicability of HMOs in opposition to this pathogen remoted from numerous anatomical websites. They discovered that HMOs disrupted the formation of A. baumannii biofilms and famous vital reductions in biofilm formation for all examined isolates.
Concluding remarks
Given the rising problem of AMR to public well being care, researchers have explored alternate options for therapeutic choices, together with HMOs and different human-derived glycosides. For instance, HMOs could possibly be exploited for his or her potent antimicrobial and anti-biofilm properties in opposition to gram-positive and gram-negative micro organism, together with the ESKAPE pathogens A. baumannii and S. aureus.

